Please note that this article was originally published on Health Rising with the title “When Retreat Means Advance: A Recovered Chronic Fatigue Syndrome/Fibromyalgia Patient Looks Back”.
During my years with ME/CFS/Fibromyalgia, I had lots of unexpected experiences. More bad experiences, more frustrations and more heart-breaking disappointments than I care to recall these days.
However, one very powerful instinct I experienced was firmly front of mind, and is being echoed over and over by others that also found a way to overcome ME/CFS/Fibromyalgia. In fact, I hear it so often when people tell of their recovery from the illness, sometimes after years or even decades of being sick, that I felt compelled to write about it to explore if it was more than an instinct, but perhaps rather an important strategy to help people with ME/CFS/Fibromyalgia get over the illness.
I suppose everyone describes it slightly differently, but as I look back, I struggle to find the words to REALLY represent what I was feeling with this POWERFUL instinct. Because for me, it was much more than an instinct, it was more like a calling, or perhaps even a compulsion, a yearning if you like. So here it is; I wanted to run away – to escape!
Okay, run is a strong word – stroll might be more appropriate given my pace during those years. But what was it I wanted to get away from?
To be frank, it wasn’t really a well-considered thought, it was more like an urge. I kept feeling like I MUST leave my home, my family, my life – leave everything and head out into the country, out into the wilderness to live in nature.
I wonder if that sounds weird to you if you have ME/CFS/Fibromyalgia, or perhaps you know exactly what I am talking about. But I have to share how conflicted I felt about this, and yet how plagued I was by this urge for the last years of my experience with ME/CFS/Fibromyalgia.
It’s fair to say that I love nature – I have loved the forest since my childhood – I love the beach – I love the mountains. But you know, I am not necessarily the camping guy – maybe a day or two and that’s always been my limit.
But my urge was to get away somewhere where there was no civilisation. No people, no TV, no anything. But besides the fact that I am married and have children, I was faced with the very stark reality that I would probably find it impossible to look after myself and provide for my basic needs. And yet, this urge continued.

I would dream of literally just getting away to live in some cabin (camping in the wild wasn’t going to work for someone too sick to get out of bed a lot of the time). Eventually, this urge was so powerful that my wife and I seriously discussed the possibility and considered our resources for me to hide away for a period of time. How long? Weeks? A month or two? Nothing was ever concrete, it was just an ongoing discussion about how this could become possible.
I never followed through with it, probably due to lack of resources and also due to fear. Given that my symptoms were so severe, that even in the comfort of my home and with the support and care of my wife, coping was difficult – going solo in the wilderness seemed crazy. But there was another fear. The fear that this inexplicable urge to remove myself from the noise, the stress, the responsibilities of normal life and the desire to be alone in complete silence with nothing to do, could perhaps be somehow dangerous for me. In fact, I felt that if I left, I might never come back, and so my love for my family prevented me from going. If I had been single, I wonder what would have happened.
This whole urge is not something I have ever discussed much with others, not during my years of illness, not in the years since I managed to overcome ME/CFS/Fibromyalgia. So why now?
Because I keep hearing others that got over the illness talk about this same urge in one way or another. And many of them have actually followed through. Not in the Grizzly Adams fashion that I kept envisaging, but in a more sensible and still supported manner.
And so I figured the question had to be asked – WHAT IS GOING ON HERE? Is ME/CFS/Fibromyalgia the body’s way of prying us out of modern civilisation? That just sounds weird!
Connecting the urge for respite in nature to overcoming ME/CFS/Fibromyalgia
In my life, a key question has always been; Why?
Why would people with such a severe physical illness, a syndrome that has dysfunctions in virtually every bodily system, possible want to seek being in nature?
What is it about nature that is calling them? Is it the trees? The air? The smells – what?
Of course I cannot comment for everybody, but in my own experience is was probably more about REMOVING myself from the stresses and stimulation of modern life. Not that I was in a bad environment or anything, the only bad thing about my environment was me and my suffering.
I didn’t want to have any responsibilities. I didn’t want to have to talk to people, pretend to be fine when in reality I was suffering more than I felt I could handle. I didn’t want the sounds, the noise, the TV, the computer. I wanted simple. I wanted …’nothingness’. That’s the only way I can describe it. I wanted not just to stop having to do things, I wanted to stop having to process things. I wanted to stop thinking about things – I just wanted to BE.
So what does all this have to do ME/CFS/Fibromyalgia? For years, I thought this whole thing was just some weird part of my life, but as I pieced together my views about the illness, overcame it and then saw many others also get over it, I started to see that this was connected to the illness. Connected to some part deep inside of me, guiding me back towards health.
The World Health Organisation (WHO) long ago classified ME/CFS as a neurological illness. And whilst long ago Fibromyalgia was thrown into the realm of rheumatology, even the American college of rheumatology now recognises the vast number of neurological symptoms including the central sensitisation involved in this pain syndrome.
Health Rising has shared many articles about research demonstrating dysautonomia in the illness, but regardless of whether you recognise autonomic nervous system dysfunction as the root problem of ME/CFS/Fibromyalgia, the point is that there is a fair amount of consensus that the illness is neurological in nature. After all, we all experience many neurological symptoms, from pain and sensitivities to light, sound and touch – to brain fog, mood alteration and sleep dysfunction. 
Clearly the nervous system in ME/CFS/Fibromyalgia is having difficulties processing sensory input appropriately, and so what would make more sense, than reducing the onslaught of information that we simply cannot tolerate?
Brain wave activity in Fibromyalgia and ME/CFS is clearly disturbed both in the waking and sleeping state. A recent study compared the sleeping brainwaves of people with and without fibromyalgia, and detected alpha waves during sleep in people experiencing fibromyalgia, something that normally only occurs in the waking states. (no wonder we feel like we didn’t sleep when waking in the morning).
And EEG studies of the waking ME/CFS brain also show significant differences.
So arousal levels, the way our brains are working and nerves are firing, is clearly abnormal both during the day and the night. (one must ask, do we really need research to ‘prove’ this? Most people with ME/CFS/Fibromyalgia experience brain fog or sleep disturbance!)
Is a health retreat a key strategy to overcome ME/CFS/Fibromyalgia?
Surely that would be a stretch of the imagination. I seriously doubt that if I had holed myself away in the woods that I would have recovered from ME/CFS/Fibromyalgia without all the other things I did to recover.
Would it have helped? Maybe, who can tell?
But when I look at the strategies that I did use, they perhaps reflect many of the experiences that such a retreat would have offered.
When I came to the conclusion that autonomic nervous system dysfunction is central to the illness causing the immune dysfunction and an extensive list of symptoms and further dysfunctions, my research and instinct identified that meditation would likely have a strong benefit. I wasn’t drawn to the process; frankly my brain felt too fried to really make any progress with such brain training exercises, and yet in my state of desperation, I persisted.
Of course, it wasn’t a magic bullet, meditation was one of many brain training and other physical strategies and treatments that eventually allowed me to make a full recovery after nearly 7 years of severe illness. However, to this day I strongly advocate this as an important foundation strategy to help people overcome Fibromyalgia and ME/CFS.
So how does meditation affect the nervous system, the brain?
Given that brain waves are abnormal in people with Fibromyalgia and ME/CFS, we can ask: “What can we do to help normalise our brain function?”
One obvious candidate is neurofeedback, where a number of electrodes are placed on our head to measure our brain activity, and some kind of feedback is given to us (most likely visually), to allow us to train our brain to produce more favourable brain waves. But let’s first look at what we are talking about with these brain waves. Here is a graphic showing the various frequencies:
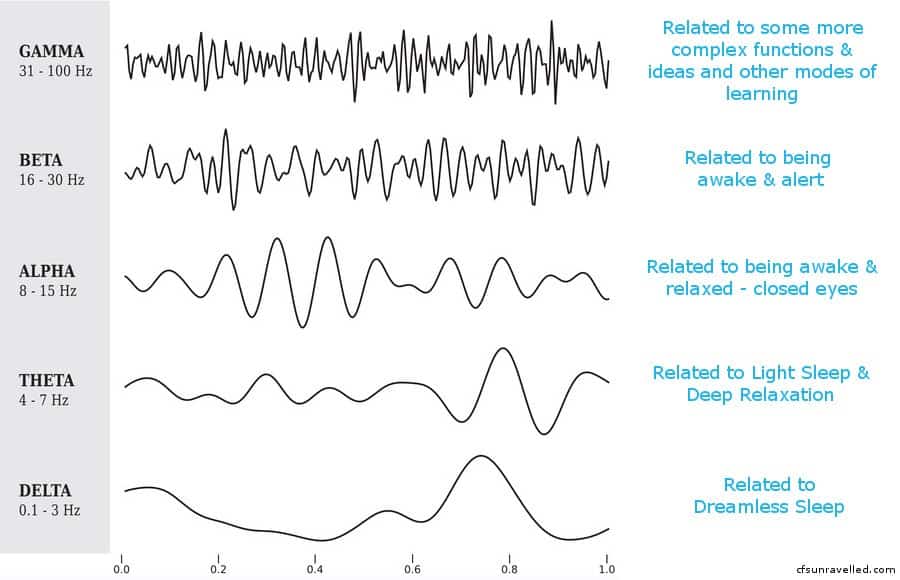
Another common brain training modality used to affect our brain wave activity, is mindfulness meditation. EEG studies indicate that our brain wave frequencies slow down when we engage in mindfulness medication. Plus, the different parts of the brain synchronize better together. (Many brain disorders are characterized not by damage to a part of the brain but by poor brain synchronization.) So it isn’t just about frequency and arousal, but also about what areas of the brain are active and how they interact. It is about a change in function!
One study found that meditators showed stronger activations in the rostral anterior cingulate cortex and the dorsal medial prefrontal cortex bilaterally, compared to controls. Both of these areas have been implicated in ME/CFS and fibromyalgia. These are areas involved in autonomic function, emotional regulation, cognitive function and memory processing as well as pain processing
So it should be no surprise that meditation has long been used to help chronic pain sufferers reduce their experience of pain and to help people experiencing a high degree of stress to cope better. Given the severity of the illness and the large range of symptoms that we experience, clearly there is much scope for people with ME/CFS/Fibromyalgia to experience benefits.
So what is the connection to that ‘call to nature’ and overcoming ME/CFS/Fibromyalgia?
It strikes me that most people that experience the illness, soon come to recognise an aversion to stimuli and an intolerance to stress. Symptoms like sensitivity to light, sound, touch (like allodynia) and even our heightened sensitivity to pain all point to highly aroused overly sensitized brains.
Meditation and focus on the breath has been shown to slow down the frequencies of brain waves. So if meditation can be used to train our brain to be less reactive, and to express more usual and healthy arousal levels during our waking and sleeping states, it would seem to be a good idea for people experiencing ME/CFS/FM. People can also use neural entrainment music (also known as brainwave entrainment), to alter the brainwaves their brains are producing (as measured by EEGs).
But what does being in nature have to do with altering brain wave patterns?
Well, it should be no surprise that many guided meditations also include sounds of nature. Sounds like chirping birds, lapping waves at the beach, trickling of water or the sound of trees swaying in the wind. These are all low frequency sounds, gentle sounds that have a soothing effect on the nervous system.
In order for us to respond appropriately to mental demands, our brains modulate activity and arousal in line with the environment and task at hand. If we need to be alert, beta waves are helpful; if we’re in high response or learning environments, gamma waves are likely to be ideal. If we want to experience sleep, theta and delta wave activity is required.
A brain that doesn’t follow these normal patterns in response to cues leads to inefficiency and frustration when we wish to perform mentally and/or when we wish to sleep.
So a normal functioning brain needs to be able to respond appropriately. Clearly just lowering our arousal, especially if we are already under-aroused, isn’t likely to be the complete answer. Which is why meditation alone isn’t the ‘cure’ for the illness.
It also makes sense to train the brain to respond appropriately when it is called into action and an increase in arousal is required. Being able to tolerate external stimuli and maintain homeostasis and a healing state without extreme shifts in arousal is critical. And so removing ourselves from stimuli that feel uncomfortable and trigger flare-ups surely must be as important as encouraging a reduction in brain arousal levels.
Perhaps the seemingly odd compulsion to get away from all stimuli and to experience the rhythms at frequencies associated with lower arousal and parasympathetic activity actually makes a whole lot of sense. Perhaps, we should all listen more to our instincts!?
Have you ever felt a compulsion to get away from it all?
Here are some images for sharing on social media:

This is exactly my compulsion. When I am well, I think I will be into walking in the wilderness and such. Funnily enough, even before I was ill, but still going through the devastating circumstances that I went through, my instinct was that if only I could get away, I could come to terms with it all.
Isn’t it interesting? I sure think that creating some space for our recovery is helpful – sometimes we can even ‘get away from it all’ whilst still at home. I never had the luxury of really ‘getting away’, so I just tried to recreate that kind of experience at home.
Yes this had been a constant throughout my illness. When I have done so I have felt a little better and more rested. It would be nice to see what would happen if I could do it for many months. When I got sick one of the first things I did although I could barely get there was head to the mountains 2 hrs away and I just jumped in a flowing river grabbed onto a rock and just let the water flow over me. It just felt helpful somehow although 1x wasn’t exactly curative. I live near the beach… Read more »
I am slowly recovering from fibromyalgia/ cfs. I believe my illness was triggered by a high stress lifestyle ( My mother in law was living with us to help babysit my young sons. My younger son was diagnosed with Aspergers. My mother in law has different values then me and it was very stressful. I was working full time as a pharmacist and our house had a mold problem.) I started recovering through mold avoidance. I went to the Death Valley California area for 3 weeks and almost felt normal 80% decrease in symptoms able to hike. We remediated our… Read more »
Hi Sue,
Thanks for your comment and sharing your experience.
It’s great to hear that you are making progress – keep going until you are fully well. ?
Totally understand the skepticism, been there myself, which is why I wrote the book to help people understand the connections.
What do you think would have helped you to overcome your skepticism sooner?
Oh my gosh! So happy to read this Dan, I have always loved being in nature but during my illness I have become obsessed with escaping! I’ve felt from the beginning that I needed to be somewhere remote and completely restorative and natural. I keep saying to my boyfriend “can we just go and live in a cabin somewhere while I recover”. Sadly like yourself I’m having to create the best I can at home. I hope that I’m at least up to a break somewhere sometime soon. My GP was saying how she wished the old fashioned ‘convalescence homes’… Read more »
I have always needed time alone in nature. I grew up on farms and moved back to a rural lifestyle when I was 30. For me, Fibromyalgia and then CFS developed early – and got a lot worse from 30 onwards. I do wonder whether having the space to get out for walks alone or with my dogs helped me to be more active than most people with Fibro. It didn’t stop all of the symptoms developing though. Now I am 4 months into recovery and we are planning our early retirement from farming, and moving to a forest area.… Read more »
Hi Ali
Yes, we need more comforts. Great to hear you making strides forward.
hi dan, interesting article.i was diagnosed with me/cfs in 2007 and I had this compulsion too. 10 years ago I actually did it. I moved to an isolated rural location in the UK and persuaded my wife to come too. however I got involved with farming and doing and never really reaped the benefits. doesn’t help that tractors and combines are often buzzing around me and I sit there seething wishing for tranquility. looks like I didn’t realise the reason why I had this urge. I still long for a life where I don’t have to do anything and just… Read more »
Thanks for sharing your experience – funny how things work out sometimes.
Hope the recovery interviews inspire and support you with your recovery.