10 years of 'success' and failure with pacing transformed:
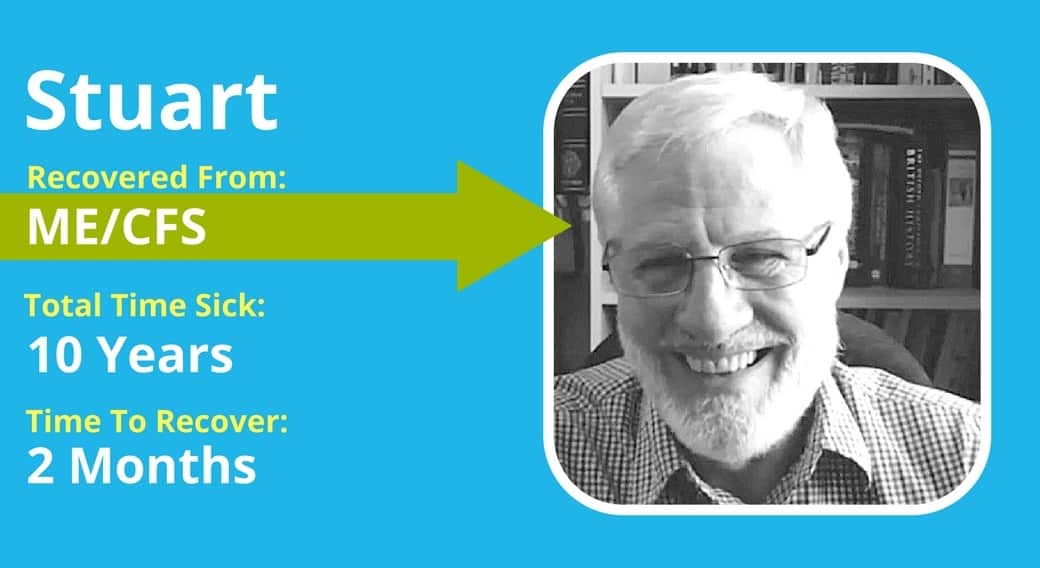
Stuart Aken heals from ME/CFS in 2 months and has stayed well!
For Recovery Story Disclaimer, please see the main page here!
Most of us have tried pacing in some form or another when we experience ME/CFS, Fibromyalgia or POTS. Either we are told about this idea, or we simply discover it ourselves when too much activity leads to crashes or flare-ups.
Stuart tells how one organisation helped him learn about pacing for ME/CFS and how it was the main strategy that helped him. In fact, it worked so well for him that he started to think he was recovered. However, as soon as he exerted himself like a normal person, he got sick again.
Dejected but not discouraged he tried again, and the same thing happened again – in total 3 times in 10 years. Then his work days changed and with that, so did his health and he recovered dramatically in “6-8 weeks”.
Listen to the distinctions in his recovery efforts, the distinctions in how he engaged in the pacing strategy and what life has been like since he has recovered. in this wonderful interview.
Transcript:
Dan: Today's recovery story is with Stuart Aken from the UK, who recovered after suffering with ME/CFS for 10 years. Stuart shares his journey and struggles with the illness, and how pacing was the only real strategy that he thought might help him. However, whilst over a period of time his symptoms reduced with this strategy, every time he thought he was well and then tried something like a normal, healthy person, he would simply get sick again and end up right where he started.
It's easy to see why people give up on strategies like pacing but Stewart felt he didn't have any alternative options. And so, despite three failed attempts to recover with pacing, he persisted. Then, his life changed and he made a sudden and robust recovery in a period of six to eight weeks. Like always, the wisdom, the important distinctions, are in the subtleties. So, listen carefully to how Stuart approached the pacing strategies and how those around him supported him in the most effective way as well as the initial choice he made that he feels saved him from ME/CFS completely taking over his life. I hope you're inspired. I look forward to your comments as always.
Today, I'm lucky enough to be speaking with Stuart from the UK, who is here to share his story of recovery. Thanks for coming to share your story, Stuart.
How Stuart’s ME/CFS symptoms started
Stuart: You're very welcome.
Dan: Yeah. Look Stuart, just for our viewers to start off with them. Did you recover from CFS or ME, it's mainly referred to in the UK or was it Fibromyalgia or both?
Stuart: It was ME/CFS, yeah.
Dan: Okay. Did you also experience a lot of symptoms, like what people describe in POTS as in the orthostatic hypotension and tachycardia, and multiple chemical sensitivities? Or was it more strictly ME/CFS?
Stuart: It was much more strictly CFS, yeah. I mean, I had other symptoms, but as you know, it's a package that you get.
Dan: That's right, a package. And not the kind of package that we normally want to get, but indeed, and in fact, I think that's one of the biggest clues. So, when did you first know that something was wrong?
Stuart: Well, I became ill with a peculiar virus in November 2002, I had to remember that. Which was a bit like flu but it had the added disadvantage. I was having problems with my balance.
Dan: Right.
Stuart: I'm the sole breadwinner in the house, or I was then. And so, I stayed afloat for a week and went back to work. But the thing never left me. And by Christmas, it was becoming a real problem. And in fact, by February, the following year, I was having days off so frequently that I actually called into the office. They said, "Hang on a minute. Something's not right here. You better go and see a doctor," which is what I did. And that started the process. But it wasn't until about maybe five, six months later that I got the “diagnosis”. And I put it in, because this isn't a diagnosis of course. I went to see an endocrinologist. He said, we've excluded everything else. So, the only thing that it must be is one of a group of he said six particular conditions which we've bunched together under the title of ME. He said, "If you don't exert yourself...that's the most important thing, just don't exert yourself." If you don't do it,” he said, "You'll be well again in a year."
Dan: Okay. Okay. Well, that's quite a nice thing to hear. That doesn't sound too bad, although, of course, it's all relative. For many people, the idea of being sick for a year, feels like an eternity and very upsetting. When did you first start getting symptoms? What month was it?
Stuart: I was sort of building towards the symptoms after Christmas really. I mean, I just felt fluish before Christmas. But after that, I started to have the typical one that we all suffer from. And that is the delayed fatigue. I thought I haven't done much today. And yet I feel really tired. Exhausted, in fact. I started to realize that it was a delayed response. I've been busy maybe two or three days earlier. And it was, I have that same form or pattern. It was at that point that I would see the doctor, you know.
Dan: Yes. And look, I guess that doesn't really make sense. That's not normal, is it?
Stuart: It doesn't appear to be. No. No.
Dan: Normally, if you get tired, you're tired the next day if you've overdone it.
Stuart: Exactly.
Dan: Not two or three days later. So, reasonably quick diagnosis. One of the things I noticed about people in the UK, they seem to get diagnosed much more easy. And when I speak to people in the US, or Australia, it seems to take like a decade or two, and even then, they don't get it sometimes. But the UK is quite on top of it. So, I was the endocrinologist that actually diagnosed you and gave you prognosis that sounded quite reasonable. So, what happened from there on? Did you follow your doctor's advice?
Stuart’s employment difficulties due to ME/CFS
Stuart: Well, because then I wasn't... I mean, I'm retired now. But I was the sole breadwinner and we had a daughter at school. I obviously felt I've got to continue to work as much as I possibly can. I continued to do that for quite some time but I was having repeated and longer and longer kind of work. Fortunately, I was working for the local authority at the time, and they're quite forgiving, shall we say.
But there came a point where my boss called me and he said, "I'm sorry. We can't continue with this." He said, "If this continues, we're going to have to take disciplinary action because you're not here often enough." And whilst I was there, I was doing the job. But he said, "You're not here often enough." And so, I said, "Oh, well, fair enough. I'll do what I possibly can." And I went in, I think it was for about a fortnight without a break, which was the longest I've done that particular year.
At the end of which I was so bad that I couldn't go into work for fortnight. I got a call from the office to go and see the... what was his name? He was the guy who looked after people who've got problems, basically. And often if you had to see him it was basically to get the sack. But fortunately, I mean, talk about good look. His wife was a sufferer. And when I told him what the problem was, he said, "Oh, right. Fine. We can deal with this if, he said, …if you're capable of doing some work, we can sort something out.” What he suggested was that I went on a half time contract.
Now, by pure coincidence, we've got a new system in place on the welfare in Britain called working families tax credit. And what that actually does is it increases your earnings. If you're after work or if you're only working shorter hours, and we work out with the reduction in tax I'd be paying and with the tax credit, I would still be able to actually exist. We'd still be able to manage as a family, on my 18 and a half hours a week. That's what we did. It took me about probably two years to find a pattern that really suited me.
And then, by that time, I tried sort of two and a half day weeks. I tried half days, you know, every day. I tried a day, break, a day, break, half day. I tried all those different patterns. In the end, it turned out that the best thing for me to do was actually to work in the mornings and have the afternoons off. At which point, I rested during the afternoons. That sort of kept me going really for the rest of my career until I retired.
ME/CFS treatments Stuart tried
Dan: Okay, very interesting. Did you seek a whole bunch of treatments? Did you seek any help or did you just go with what the doctor said that you should just rest, which obviously you didn't manage to do per se.
Stuart: Well, because I had loads of symptoms, there were times when obviously I would see the doctors. I was a patient and part of a large practice at the time with about 12 or 13 doctors. One of whom, was probably quite sympathetic, and also recognized that the medical profession didn't know what was going on. So, she was quite open and honest with me. And it was she, I think, who actually put me in touch with an organization online called Action for ME.
And so, I actually came back home again and went online. And they sent me loads and loads of information. Because, as it's common in the situation, I couldn't really read off the screen very easily. Problem. So, she sent me all this stuff. Another period of time, after having ready, I discovered there were various things that I could do that might be helpful. And so, I just tried various different routes. I didn't get any medical help, other than painkillers, because in common with everybody, you get paid. In my mind, my particular pain was from my shoulders down from hips. The whole trunk was with pain and after a while painkiller didn't make any difference anyway so I stopped digging. I was helped much more by this organization than by anybody in the medical profession.
Dan: Okay, yeah. It's great to get some information of what are some options. The internet is a wild place. It's difficult to read through all these suggestions. Everyone has an idea. Everyone has some sort of a cure that they think will work for you.
Stuart: Yes.
Dan: It's always focusing on symptoms. It's never really focusing on the syndrome.
Stuart: That's right, yeah.
The different ME/CFS symptoms Stuart experienced
Dan: Speaking of symptoms and syndrome, the package that you mentioned earlier, can you sort of share a little bit about the range of symptoms that you actually experience and how that changed over time?
Stuart: Well, some of them were intermittent. Some of them were constant. Some of them were there for a short while and then went. Some of them were for a longer time and went. So, I mean, I've made a list because to be honest with you, I don't know about you, but I'm over it now. That's in the past. I try not to think about it.
Dan: Absolutely. Absolutely.
Stuart: I have to revisit my book, to remember what it was.
Dan: Yes.
Stuart: And basically, I mean, the delayed fatigue was the most obvious thing. Pain, as I said, the whole much, my body shrunk. I had tinnitus, which was a real problem because I also have a slight hearing loss as well. That was a real... Particularly because the job I was doing, involved me sitting in an open plan office with a headset with only one ear on because I had to be able to hear what my colleagues were saying. And I was on the phone dealing with technical issues to do with business rates, which is a form of taxation in the UK. I don't know if you pay it in Australia, but it's a type of taxation. Quite complex and very technical. And so, I was dealing with people's issues on those things. So, that was one of the things. So, the tinnitus obviously wasn't really very helpful.
Dan: Did that come on with the illness or was that there beforehand?
Stuart: It slowly developed. It just slowly developed. It stayed with me for, I would think, probably seven years. And then went again. There's no apparent reason for any of these things.
Dan: So, Tinnitus, pain, fatigue.
Stuart: Yeah, I had night sweats. Now, that was actually something which caused my wife and I quite a bit of amusement in certain ways, because she was also undergoing the menopause. Women in the middle of menopause get rather warm. So, sometimes, we're two radiators sleeping in the same bed. It was quite amusing. But we were able to joke about it, fortunately enough.
Dealing with the embarrassment and confusion of ME/CFS
Dan: Well, it's great to bring humour when you've got such a difficult time. It gives you a little bit of release, doesn't it?
Stuart: It's essential, I think. Yeah.
Dan: I lost my humour after several years, to be honest. It took a while to come back. So, it's great that you managed to maintain it.
Stuart: It's hard though, isn't it? But obviously, the night sweats didn't help the sleep. I think I had broken sleep throughout the entire period. I don't think I had a good night's sleep at all ever during the entire period I was ill. Some nights were better than others. So, that was another symptom.
I suffered from temporary impotence, which I think was more to do with energy than anything else. I suspect a drop in confidence because obviously, you know, you're no longer performing the way you normally do as a man. I think I had that effect.
And a couple of things that were actually for me the most troubling, one of which was loss of short-term memory. So, I'd be talking to somebody in the office, who I'd known for years, and couldn't remember the name. I mean, I've known it then. And two seconds later, I couldn't remember who they were. That was really, really distressing. But the other aspect of that, which I found quite difficult to deal with was, I'm a writer. And although I wasn't writing as a professional, I was writing in my spare time. And so, words are the things that I deal with an awful lot. Obviously, words are really important to me. And I would find that I was talking to somebody, often with a very technical issue, and suddenly couldn't remember the terms that I needed to explain what I was trying to say. And that was very distressing. And actually, added to the stress, which probably was the cause of the problem in the first place.
Dan: Yeah. Yeah. It's a very difficult and distressing thing when we lose our ability to be articulate to communicate. And nothing worse than not knowing someone's name that you know you should. I mean, it's almost scary, isn't it really?
Stuart: It is, yeah. People that I've been working with for years and who sat opposite me. I am with them all the time.
Dan: Believe me, I forgot the names of people that you cannot ever imagine finding an excuse forgetting. It's like I'm almost embarrassed to talk about it even now, after all these years. You know what I mean?
Stuart: It is embarrassing.
Dan: It's crazy. Yeah. So yeah, go on. Let's get through.
Stuart: That's also caused a certain amount of confusion obviously. There were times when I felt confused for reasons that I didn't understand. I just felt that sort of general sort of sense of confusion. Usually, that happened at work but sometimes at home.
And then, the thing that I think was also slightly concerning was, I've generally in life been quite laid back. I've been a sort of, you know, "Okay. So, yeah. We'll deal with it." But I found that my anxiety level rose quite well, exponentially. It was amazing, really. And that is the one factor that's remained since I've been recovered, is that I find that I have an increased level of anxiety. And from what I remember in the past, you know, because people used to say I'm so laid back and fall over, but there must be a better way to describe me. But now I find silly little things. You know, like, if I've got a meeting or an appointment, I start to feel slightly tense about it. It was always something which didn't matter too, which you know, we will get there you know. That is a hangover from it, if you like, but nothing as intense as it was when I was suffering.
Dan: What did that make you think was going on? Because I mean, obviously, you were lucky enough to be diagnosed with ME.
Stuart: Yeah.
Dan: So, I guess you didn't get the “oh, you're depressed or you're anxious or it's all in your head”. I'm assuming you didn't get too much of that by the sound of it.
Stuart: I was depressed. But as I said to the doctor when she said you're depressed, I said, "Well." I said I've been active all my life. How would you feel if the only way you deal with your life was by working, sleeping badly, and resting? That's it. That's your life. Nothing else.
Dan: Yeah. Of course, it is depressing, isn't it?
Stuart: And she said, yes. Depression is a symptom of ME.
Dan: That's it.
Stuart: It's not the cause.
Dan: Yeah. And this is the thing that many people feel frustrated about. Of course, it's quite natural and normal to feel depressed but I guess it's important to have it acknowledged and recognized as something else going on. And that you actually, you're really physically ill. It's not that you're just feeling down.
Stuart: I actually suffered from clinical depression as a teenager to the point of being suicidal at one point. So, I knew what symptoms are. That was something we just did a couple of years. Circumstances change that. I understood the dangers. I understood the symptoms. I understood how to deal with it. And the last thing I wanted was drugs to deal with it because I'd been on those before. No way. Thank you. I'm not going through that again.
But it wasn't... I wouldn't want to say it was a major problem because I think I recognized it as a symptom, as a response to the condition to the way in which it was affecting my life.
Dan: A natural, normal response.
Stuart: I think I was able to sort of, in a sense, rationalize it, you know, which made it easier to deal with. Then, apart from all that, there were some random symptoms. So, on odd occasions, I would have a sore throat that would last about three or four days for no apparent reason and then go again. Headaches, I've got headaches. I actually got a significant increase in the number of migraines. I suffered from migraines all my life but only very, very rarely. I was thinking, maybe six or seven in a week.
Dan: Wow, that's huge.
Stuart: A lot, yeah. And I was able to get some medication for that, which was helpful. Sudden bouts of indigestion for no apparent reason. It didn't have anything to do with what I've eaten. No logical sort of explanation for it. And bouts of breathlessness. Rather alarming, sudden loss of total body strength. I would actually be in a situation where I was walking somewhere and I would literally fall down.
Fortunately, I was really fortunate that only once did that happen on my short walk from the office, to either the car park or the bus station, which is eventually I took the bus to work. And unfortunately, at the time, I was really, really close to a bench and I just collapsed onto the bench. But it's quite alarming because there was no warning. It's just very suddenly. And I had visual disturbances, which were quite disturbing, quite odd, which made reading and so on quite difficult. And again, sometimes only for very short periods but they were there. And then finally, of course, I got quite a lot of pain in various parts of my body for no apparent reason. Most notably, in my big toes.
Dan: Yeah, interesting.
Stuart: It was slightly odd.
Dan: Hard to explain that one away, isn't it?
Stuart: Yes, you know.
Dan: Yes, quite it is. Okay. So, I mean.
Stuart: So those are my symptoms, yeah.
Dan: Obviously, it's very difficult to go through this. And you mentioned being depressed and having some anxious feelings. But I mean, as time went on, and obviously the 12-month period went past, you struggle for work. I mean, how did you manage to cope with your life? How did that whole thing affect your life?
How pacing strategies for ME/CFS help Stuart find a temporary recovery
Stuart: Well, I've always been an optimist. It's been something which has been with me all my life. And my wife and daughter were incredibly supportive and nursed it. I mean, my daughter was only nine when it started with it. And so, she didn't really fully understand, obviously, but she accepted it. And my wife just knew that I was ill, you know, that she'd known me as a fit man. And she just knew immediately. In fact, it was she who sort of pushed me to call and get some sort of treatment. But so supportive. I sort of developed an attitude that, "Okay. I woke up this morning and I can move. I can get out of bed. That's a plus." And I looked for everything that was positive.
What I also did was I took advice from the Action from ME Literature. I've tried several of the different approaches that they made but the one I actually hit on as being something which seems to work for me was what's called Pacing, which I think you're probably aware of. I tried that. And on either two or three occasions, I can’t remember now, I was convinced that I'd beaten the condition and carried on. I physically got better and carried on and started to live a normal life and bang... straight down again.
Dan: Yeah, that's very obvious way of saying... How long into the illness was that you had this turnaround? I mean, it was specifically the pacing that got you there? And how long did that take it?
Stuart: I think the first time because obviously I did a period of experimentation finding out what worked for me and what didn't. So, I think it was probably about four or five years in, that I got the first temporary recovery.
Dan: And how long did it take to come? I mean, was it... Like, did you do that over a period of weeks, months? A year?
Stuart: It was months.
Dan: Months.
Stuart: It was months. Yeah. I mean, I would say probably 9-10 months, that sort of period before I felt that I was sort of back to normality again. But as I say, I was fooled by that. And that happens about two or three times.
Dan: How long did your recovery last each time?
Stuart: Oh, weeks.
Dan: Weeks. Okay. All right. But I mean, obviously, it was getting better over those 10 months, let's say?
Stuart: That's right. Yes. Oh, yes it was certainly improving.
Dan: Improving all the way. And then when you had another flare up, did you just go back down a little bit or did you go really all the way down?
Stuart: From the fatigue point of view, I went all the way back down again. But the other symptoms were diminished.
Dan: Okay, that's interesting,
Stuart: So, that was one of those occasions that the tinnitus stopped again, which was great. You know, that was helpful. But the fatigue and the short term memory and periods of confusion, they came back almost immediately. You know, so.
Dan: Now, obviously, I guess, you must have been very encouraged that first time, especially when you started doing this pacing.
Stuart: Absolutely. Yeah.
Dan: I guess it was in line with what the doctor said to you. Because in the beginning you said, you need to rest. And obviously, pacing is a form of resting.
Stuart: Yeah. That's right. Yeah.
Dan: So, when you heard about the pacing and you did that, have you tried a lot of other treatments before that?
Stuart: There were other things that were suggested. Some of which I just didn't think were things that I could do at all. To be honest with you, I now can't remember what they were.
Dan: Yeah, that's fine. That's fine.
Stuart: There were two or three that I did try. And as I said, I honestly can't remember the word out but there were recognised attempts to get better. They just didn't work for me. For one reason or another. Either because it was impractical or because it just didn't suit my particular condition and circumstances.
Dan: So, when you then first... Sorry, go ahead.
Stuart: I said the pacing did seem to work for me. And it was noticeable. That was the point. I could actually feel myself improving. But judging when to stop an activity, and how long a rest to have afterwards was the most difficult part of the whole thing. It took a long time. I mean it took me quite a few years to work out what was the best combination, you know, and how it worked. And of course, it continually changes...
Dan: I was going to say, yes…
Stuart: As you are improving. You can do that little bit more.
Dan: That's right.
Stuart: So, you really had to become conscious of your body and how you felt and what you could and couldn't get away with basically.
Dan: Before we get to that. And I think that's a... Perhaps you have some really great insights here, you know, so I want to explore that a little bit more in a moment. But I guess my first question is, when you did all feel well and suddenly feel really good after 10 months the first time and then suddenly you go back down, I mean, what are you thinking?
Feeling depressed with ME/CFS after relapse and finding a way back
Stuart: I was severely depressed for a while. And I mean, there were a couple of sorts of black days when I thought this is never going to go away. I'm going to be like this for the rest of my life. But as I say, fortunately, I am an optimist. And obviously, I'm not very bright. Because, otherwise life experience would suggest that there's no good reason to be. I am and I always have been. I continue to be optimistic.
Dan: Good for you.
Stuart: I think that positive approach to life has really been helpful for me.
Dan: Absolutely. Absolutely. You know like, reflecting my own experience. I'd like to say I'm an optimist. But I'm one of those realists. See, I can't bring myself to say the word because I don't like it. And I guess the reason why I don't like it because I've seen the power of optimism. I choose to do my best to become more optimistic all the time but my natural default was to be a realist. But my wife is an optimist. Yeah.
Stuart: Yes.
Dan: And even in the face of all logic telling you that there is no hope, this makes no sense, there's no way you can get better. Because, you know, I have proof that you can’t get better after so many years doing everything in it. All my research and all this kind of thing. Some people are optimistic in the face of that. Now, I always admire that because it makes no sense to me. And yet, it's still so helpful. So, I love how you're bringing this up. So then, how long did it take you then to have another go at the pacing, after the first setback?
Stuart: I would think about 18 months.
Dan: Eighteen months. You didn't want to straight away?
Stuart: I never actually stopped. I'm sorry?
Dan: Yeah. So, you didn't want to try straight away? Or you basically...
Stuart: Well, I gave myself about a fortnight to three weeks to be honest with you. And it started again from the beginning. There's a very short period of activity, long periods of rest. And I just built it again.
Dan: Okay. And then how long did that take? Eighteen months?
Stuart: I had a second period when I thought I was recovered. But you see, I'm not very bright. As I say, I obviously didn't learn from the first time and went straight out. I thought, "Right. Great. Get on with it. Go and get to the end of it." And of course, down again, straight away.
Dan: Right. Right. Straightaway. So, your period of weeks basically. And then?
Stuart: Oh, yeah. Days really rather than weeks.
Dan: I mean, how does that happen? I mean because you're pacing and pacing and pacing, do you then one day say, "Hey, I'm fully well and now I'm going to go run a marathon or?"
Stuart: Well, not quite as bad as that, but I did go out and do jobs that had been needing doing around the house. Quite heavy labour and gardening jobs that sort of thing.
Dan: Yeah. Finally, you feel good enough. I'm going to tackle it.
Stuart: Yeah. I thought, yes, great. I'll help in the house.
Dan: Yeah. I understand. I totally understand. Okay. And then, third time lucky. Is that what happened?
Stuart makes the link between ME/CFS and stress
Stuart: I think I had a third time where I failed again. Then, what actually happened was in 2013, I was 65, I retired from work. Within weeks, I was recovered.
Dan: Wow.
Stuart: And I've never been otherwise. I am absolutely positive that the major problem that I had was stress. And it was mostly work-related stress.
Dan: Right. Right. Well, that's the interesting thing because you know, when you're speaking on the telephone to someone, it's a very unnatural way of communicating.
Stuart: Oh, yeah. Yeah.
Dan: Because so much of our communication is obviously nonverbal. And when you don't see someone, and you are talking about something technical, you really have to put yourself through that fun, don't you?
Stuart: Oh, yeah. Absolutely.
Dan: Besides, you always have to project yourself and it's very stressful.
Stuart: Yeah. And often there weren't very nice people I'm afraid, lots of people I was dealing with on the phone.
Dan: Very angry people.
Stuart: Well, we were dealing with more like, you know what people are like when they are dealing with money.
Dan: Sure. Sure.
Stuart: And although I was trying to help, there are obviously situations in which I couldn't do what they wanted me to do. Mostly they are business people I was dealing with, obviously. Some of whom, to be honest with you, could not have run a party in a brewery. They were just so incompetent. Unbelievable. And others of them were sorts of people who had done very well in business but whose attitude to other people was they were dispensable commodities. So, there was always that sort of difficulty.
Stuart: There was also one other thing which I had a particular colleague at work who was constantly, and I do mean constantly talking. So, there was never ever a break from that voice. And just across the desk, you know. And that, of course, was very difficult to deal with when you're on the phone with somebody else, you know, particularly with things you are hearing.
Dan: Yeah, absolutely.
Stuart: Because you'd drown out so I really had to concentrate all the time. And once I was listening to, you know. So, I think once I got rid of that aspect, and I think also the fact that I was dealing with a law, a group of laws, with which I had great difficulty because I thought that they were frequently unfair and not helpful.
Dan: And you had to enforce or represent them.
Stuart: I had to, yes, because I was working for the organisation, you know, and so on. So yeah, I think all those things put together, put a great deal of stress on me. And once I was released from that, I very rapidly, again using pacing but so much more effectively, very rapidly recovered to the extent that a short time after I retired, started to go and look for a new place to live, somewhere. I was actually able to catch up on those 10 years of work around the house to get it prepared, ready for sale and so on.
Dan: Okay, so you were sick for 10 years?
Stuart: Yes, 10 years. Yeah.
Dan: I guess, obviously, seeing how you stopped working and suddenly recovery not only came quicker with the pacing but it became robust and lasting. Obviously, you made that connection to stress. Let me ask you, have you made that connection that it was stress before that? Did you think it was stress during those 10 years?
Stuart: Yes.
Dan: Why is that?
Stuart: Yes. Unfortunately, I'm in a position where I couldn't actually do much practical about it.
Dan: Sure. I understand.
Stuart: Sorry, you froze.
Dan: Yeah. Sorry about that. So, I wonder why that was. Was it because of the way your illness started? I mean, how did your illness start? What happened in the 18 months leading up to the onset?
Stuart’s lead up to ME/CFS onset
Stuart: Well, the onset as I say, it happened as a result of a virus.
Dan: Yeah. Did anything else happen in that lead up? Was there a change to your work of circumstances? Did you do any physical events? Was there anything else that happened in that 18 months?
Stuart: I'm trying to think of 2002.
Dan: Major events.
Stuart: I had the usual sort of what I would call family and domestic stresses that you have, you know. I mean, people die. My father wasn't well. My stepmother wasn't well. I have a brother who's got Type I diabetes. I mean he had always been remarkably active and so on but, you know, at the same time you're conscious of the fact that it's a serious illness.
Dan: Yeah, for sure.
Stuart: So, those sorts of things had always been there in the background, as they always happen. I think probably one of the events that was possibly an important aspect was earlier I'd had... In 2000, when it's, in fact, on the 17th of December 1999. I was made redundant, just before the millennium. I'm trying to find work at that particular time. I was one of 14 in the company that was made redundant. One of them was actually managing director of one of the brands. I found that very, very distressing as you can imagine. I found a little job. By February I think I was back in working.
Dan: How did you adjusted in your job? Was it difficult or easy?
Stuart: It wasn't easy because I was working in a call centre. Initially selling stuff, and then dealing with customer complaints and so on. Many of which were justified. And so, when this job with the local authority came up, I thought, "I'll have that."
Dan: And then, how was that? Was that easier or was it still difficult?
Stuart: It was easier than working in the call centre, yeah. I got the call centre job because I'd been a call centre manager, and team leader of it. It was such a natural thing to do.
Dan: Okay, and then how long were you in that job before you got sick?
Stuart: It was 2003 when I was diagnosed. It was in February. And I started in August 2000. Yeah, by 18 months.
Dan: So, the reason I asked, many people find that shortly before they get sick, there's something that happens. They get, you know, an immunization, they go and do a sporting event that's very severe. They have a death in the family or... Something often happens. So, I was curious if you felt there was something like that sparked. But it doesn't sound like anything obvious.
Stuart: Not an immediate event in that sense. I think it was a build up.
Dan: A build up. Yeah, it's like the frog in a hot water. It sits there because it keeps getting warmer and warmer and warmer and suddenly, he's boiling and he never jumps out. So, now when you went to, after you retired and then you were pacing, was there anything else besides pacing that you think have come part of your lifestyle as part of your recovery strategy, or was it just the pacing?
Stuart’s explains ‘How I recovered from ME/CFS’
Stuart: I think it was the combination of the pacing and the fact that I was no longer stressed by work. I think it's those two combined that actually put me at the top and allowed me to completely recover.
Dan: Did you do any sort of active strategies to manage stress or relaxation? Like, some people pray, or some people do meditation, or anything like this kind of thing?
Stuart: I have to be honest, no, I didn't. No. I live a lot of my life in my imagination. I'm a writer. So, even when I'm tired, there are stories going on in here. And so, I've always been a daydreamer. In a sense, that's been my escape from reality. I think that's been a useful defence against some of the things that life throws at you. Once I retired, of course, I was able to spend a lot more time writing, and therefore letting this creative impulse out in a positive way. I've published about 12 books now.
Dan: Fantastic. Amazing achievement.
Stuart: So, it's really helped. That has been, in a sense, it's been my blessing, you know, the fact that I can convert these things that are going in my head into words on paper.
Dan: Absolutely.
Stuart: And write stories.
Dan: Now...
Stuart: And also.
Dan: Go ahead.
Stuart: As you said, as a writer of fiction, you live vicariously a lot of the time. So, you're living through the lives of your characters. So, again, it sort of takes you completely out of yourself.
Dan: It's a beautiful escape.
Stuart: Into an entirely different world. Yeah. Yeah. Very useful.
How Stuart made pacing work effectively for ME/CFS
Dan: I'd like to explore a little bit about the pacing. I wonder, is there any insights you think you have to offer for people about how you managed to find a way to effectively pace because, you know, it is a challenge, as you described.
Stuart: I wish I could say that there was some sort of lightbulb moment that came but it wasn't like that. It took a long time to determine how much I could do at any one given time. And then, how much of a rest I needed afterwards. But I followed that pattern quite religiously. So, if I had been active, I always made sure I had a rest.
Dan: Even if it didn't feel like you needed it.
Stuart: Even if I didn't feel as if I need it, yeah. Also, the very least was at least as long as the activity had been. Generally speaking, longer. But you know, that was the least I would allow myself. And I would measure. And when I was resting, I was resting. I literally was lying on the settee. I didn't read. The only thing I did was either listen to music or watch daytime television. Thank heavens for the remote control because it was so boring.
Dan: Yes. Yeah.
Stuart: I could just change.
Dan: Yeah, because easy... because reading... I mean, depending on what you read, you can read something for escapism, but reading can also become very cerebral. Especially if you're a writer, then even fiction can be almost like work because you're interpreting and looking at what you're reading, isn't it?
Stuart: Well, I always review. If I read a book I always review.
Dan: Yes. Yes.
Stuart: I'm trying to help my fellow authors. And so, to a certain extent it is work.
Dan: Tell me. Is there any sort of...? Did you go back and tell your doctor that you had recovered?
Stuart: Only when I had to go to the doctor.
Dan: And what did the doctor say?
Stuart: I do tell him something is a matter, of course, you know.
Dan: Yeah, for sure. So, what did your doctor say?
Stuart: She was delighted.
Stuart’s finds new work and life after recovering from ME/CFS
Dan: Great! Okay. Fantastic. And then, so tell me, is there any sort of particular things that you've done since you've recovered? Like, you are feeling well again, that perhaps you thought you'd never do. You know, moments where you pinch yourself, "Oh, my goodness. I can't believe this is happening."
Stuart: Well, as I say, we moved house a short while. We actually came to this house we're living in now in January of 2015, which was about 18 months after I retired. Amongst other things, I did a patio with concrete slabs, you know, was with slabs. Completely demolished the jungle that … I have a slope at the bottom of the garden, which is a... it's I would think about a one in three slope. It's very steep. So, very difficult to work on. And it was covered in weeds, brambles and other things, and I cleared that. I discovered there were some steps down there. We cleared all that and laid a garden path, built garden shed.
Dan: Were you not scared doing all these things, Stuart? I mean, you know, when you were sick all those years, and it took so much from your life, and you had all those setbacks every time you went to do something three times, yes? I mean, you clearly got very depressed and down when you had these relapses. I assume that doing your years of illness, you were very scared of your symptoms. Would that be a fair thing to say?
Stuart: I was concerned that they may never go away. That was my real fear.
Dan: So, whilst you were sick in those 10 years, I mean, how did you feel about the idea of doing these heavy physical things? Did that not give you some fear about doing those sorts of things?
Stuart: No, I look forward to it.
Dan: But even though you... because you had these repeated bad experiences. Didn't you think, "Oh, my goodness."
Stuart: Yeah. But as I say, I'm an optimist.
Dan: That's interesting.
Stuart: Pretty dense really. Don't learn from experience.
Dan: Okay. All right. No.
Stuart: Well, I do but you know. It's simply with being positive about things. I'll be absolutely honest with you. Even now there are odd times when I think, "God, I hope it doesn't come back again."
Dan: Of course.
Stuart: But very, very rare. But then, apart from doing the stuff around the house, I think my sort of real achievement was when we first moved here, we were watching an event that happens every year in England, called the Great North Run, which is a half marathon, where up to over 50,000 people run 13 and a half miles, mostly for charity. And I had been so helped by... actually, ME. I thought, "I'm going to raise some money for them." I applied to go and got accepted in the ballot, and then start your training. And then in September, I ran the Great North Run.
Dan: Well done. Well done. How awesome.
Stuart: I have a problem with my knees. It's about 10 miles out. I thought, I knew I have to stop running quite here. I'm going to have to start walking and running because otherwise I will not make it to the finish line.
Dan: Yes, yes, yes.
Stuart: But I did it. I did it in two hours and 47 minutes which is quite a long time but I was really pleased.
Dan: Absolutely. And obviously, next day you felt absolutely tired. But, so what? Right?
Stuart: But naturally.
Dan: Is that a different feeling? I remember feeling absolutely exhausted on several occasions doing some ridiculous things and going, "Oh my goodness. This is what people call exhaustion." It just made me giggle.
Stuart: Yes, exactly.
Dan: This is not exhaustion. This is like I feel energized in comparison. So, it's interesting. I love how you said that you never developed the fear of doing things even though you had these terrible negative experiences and how you used optimism about that. I think that makes it quite unique because many of us, you know, keep getting these experiences where we do certain things that flare us up and make us sick. And then, we get quite fearful of those things because that's what we get sort of taught. Did you find a way any other triggers besides physical activity in particular that used to make your condition worse or gave you those setbacks?
Stuart: No. As I said, I'm confident now. Looking back with the benefit of hindsight, that the major contributory factor were work-related stress. I think everything else was an add-on, to be honest with you. So I think that there's some sort of basic problem that occurs when you've got ME. I believe it's the hippocampus, I think. This is our control centre, which ceases to operate under normal circumstances. I think what actually happens from my experience is that stress is the thing that's causing the real problem. And all the other things are symptoms. It's really what's happening is your body is saying "Stop. You need to rest. You need to break away from this."
Dan: I think this was important for anyone listening that the word stress can mean lots of things. I mean, obviously we're talking about, I suppose what we would term a psychological or mental stress. Yeah. But people can also have emotional stress. Obviously, once we get sick, there's plenty of that. But sometimes for people, it's actually physical stress. Some people will have a surgery or childbirth or an accident or all kinds of things. And the body doesn't really differentiate between a psychological stress or physical stress. And so, it doesn't mean that the illness is in your head. Obviously, the illness is very real but it just means that that’s something that triggere it. What would be your advice to people, people who are still sick? What would be best advice to someone who's listening who's still unwell?
Stuart emphasizes how the support and love of his family helped him overcome ME/CFS.
Stuart: It's so difficult, isn't it, because I think we're all individuals. Again, looking back, I think that probably the most important things for my recovery were my positive attitude, which I was managing to maintain, regardless, most of the time. Obviously, I said, there were times I was depressed. But that positive attitude was always there. And so, I've always had hope. I'd always had a determination as well to get better. But also, the support. And in my case, that was from my wife and my daughter. I can't stress enough how important that was. The fact that they did everything in their power to support me, and to maintain a belief in me and maintain their real love and care for me all the time, right the way through, never wavered at all. I think that was so important to my recovery.
Dan: I mean, it's quite amazing, you know, because I think a support person feels a fatigue also too. I mean, when...
Stuart: Oh, absolutely. Yes.
Dan: I think anyone can support someone for a week or two weeks. You got a bad flu, "Hey, I'll drop everything for you." But when we extend to months, and months turned into years, and years turned to decades, it's like, how can you keep hearing the same sad story and the same moaning and complaining and the same problem? Because nothing's changing. It's a broken record, isn't it? I mean, obviously, optimism is fantastic. But do you think your wife used any other strategies to be able to maintain this kind of a positive attitude?
Stuart: Well, if she did, she didn't talk to me. I mean, she's an intelligent lady as my wife. She's bright and caring. And actually, generally speaking, not an optimist. She's very much a pragmatist.
Dan: Yes, a realist like me.
Stuart: I mean, of the two of us, you know, I'm the romantic.
Dan: But she dug in and became an optimist because the pressure was on and she thought, that's the way to go.
Stuart: She's also one of these people who's very determined. She sets herself for tasks, she does it. And I think that one of the things that kept her going, was her belief that I would recover. And that she would do everything in her power to help me to do that. And everything in her power to help me, not everything in her power to help her. It was to help me. That really, really did sure.
Dan: I mean, wasn't for both of you that the whole way through, it was almost like, it's just going to go away. It's "I'm just going to do this pacing. That's what's going to get me." Or did you feel like you were distracted by looking at a whole bunch of other strategies, like, you know, treatments of symptoms, and all this kind of thing.
Stuart: Only in the early years. After about three years, I'd settled on the pacing. And we decided that's the route we would take,
Dan: Because you saw some kind of benefit.
Stuart: Yeah. And Valerie had also read the literature, so she understood it as well. She was like a monitor. She saw me doing something, she would say, "That's enough. Go and have rest." And on occasions, I mean, because obviously she wasn't always there. But on occasion, she would come and say, "It's not time for you to get up yet. Lie down again." It was that sort of situation. So, it wasn't just me monitoring it. Valerie is monitoring it again as well. And she's always had an ability to tell whether I'm well or not without me saying anything.
Dan: I totally know, yeah. Did she say that she could see it in the eyes or?
Stuart: Oh, yes, yeah, yeah. In the eyes. And also, I used to go quite grey sometimes. I was never conscious of it. But she'd be able to tell how I felt by the level of colour. And she was always right.
Dan: Sometimes our partners... Something that my wife used to say that she could see the eyes would sort of become glassy. She'd say they just look different. You're trying to put on a brave face, but they can tell.
Stuart: Oh, yeah. I could never fool her.
Stuart’s message to others with ME/CFS
Dan: Look, thank you so much. Now, being a writer that you are, you of course shared, you wrote about your experience. Can you show us a copy of your book and what it's called?
Stuart: It’s a...,
Dan: M.E. and me, Chronic Fatigue: My Recovery After 10 Years.
Stuart: I looked online first to make sure it was a unique title.
Dan: Yes. So, what did you write about in your book?
Stuart: It's effectively, I mean, the subtitle is Chronic Fatigue: My Recovery After 10 Years, because what I wanted to do was give people an insight into what the condition entails, how it affects your life and those around you. But also, more than anything else, I want to give people hope, you know, sufferers in particular and carers that there is the possibility of recovering from this condition. I know not everybody can. And I mean, I was really fortunate because I was never bedridden. I think once you're bedridden, I suspect that's a real problem because how would you pace if you're bedridden. How can you do anything at all?
I wanted to try and get across to people how important it is, first of all, to accept the condition. I had a work colleague, a lady, who actually went down with the condition about seven or eight months after I did, but she refused to accept it. She's a real party lady. She started coming to work in her slippers because her feet were so painful. And you could just see her deteriorating. And within 18 months of the declaration, she had to take medical retirement because she couldn't work. Full stop.
Dan: Yeah.
Stuart: And, you know, when you see that sort of thing, you think, if she just accepted that she had a problem, she might be fine again now, you know. But she isn't. I know she isn't. But if she had accepted it, you know, she might have recovered as well. I think that's really, really important. Difficult but I think it's important that you do accept. The way in which I looked at it, was if I continue ignoring this condition, it's going to get worse. And as soon as I learned about what it really was, I thought not only is it going to get worse, but it's going to not stop. It's going to just continue forever.
So, I thought what is the best strategy for me to deal with those things that matter to me? Like looking after my family, doing my writing, those things that mattered. What's the best strategy? And I thought, well, the best strategy is to do whatever I possibly can to recover. And so, that was always there at the back of mind.
Dan: So, you speak about acceptance. And pacing, I guess.
Stuart: Yeah. Yeah.
Dan: Fantastic.
Stuart: It worked for me. I know it doesn't work for everybody.
Dan: That's fine. That's fine.
Stuart: But I found that particular process works really.
Dan: Well look, I think it's fantastic. I really appreciate you sharing your story and giving hope to others and showing that recovery is possible. Now, how long have you been recovered now?
Stuart: Well, I retired in May 2013. Now in 2017, and I would say that I was convinced that I recovered within weeks, a month and a half, two months maybe of retiring. I thought, "Yeah. I'm okay."
Dan: And you felt it would stick that time too.
Stuart: Either relapse.
Dan: No, nothing.
Stuart: I've actually gradually got better. I mean, obviously age is now... because I mean, I'm 69. So, obviously that's making a difference. There are certain times the body starts to deteriorate. But I had a really sort of physically active teenage years. I mean, I was a boxer. I played rugby. I did cross country runs. I did circuit training and all sorts of things, you know. So, I was really, really fit as a teenager.
As a young man, I played badminton and various other things. So, I've always been active. I did a half marathon in 1983 as well for a local charity in a different part of the country. So, I've always been active. I think that in itself has given me that sort of core strength, if you like, that core fitness. And I'm maintaining it now. Now, I do at least 20 minutes of mixed aerobic and flexi exercising three times a week. And my wife and I, we live in a place called the Forest of Dean, which is a nice hilly area cloaked in trees. And within 100 yards of our front door, we're in the forest. And we walk there every day, often three or four miles.
Dan: That's great. That's great. Well done for sharing your optimism and for sharing hope. I appreciate you sharing your story.
Stuart: Thank you very much indeed for this opportunity to at least hopefully give people some further hope.
Dan: Absolutely. Thank you, Stuart.
Stuart: Yeah. Thank you for doing this. Thanks.
To learn more about Stuart Aken you can visit his website here: https://stuartaken.net/
He has written up his thoughts about the illness and his experience of recovery after 10 years of illness with ME/CFS in his book M.E and me: Chronic Fatigue: My Recovery After 10 Years
Please leave a comment at the bottom of the page!
Here are some social media images for sharing:







Hi, Dan. Thanks for this opportunity to tell my story and to spread some hope for those who continue to suffer with this dreadful condition. I really appreciate your care and the professional manner in which you’ve produced this piece. Let’s hope some of my optimism will rub off on others and help them manage their condition and, who knows, maybe even recover.
Thanks for sharing and inspiring hope for recovery from M.E. Stuart – people really loved your humour and happy manner. 🙂
What a fantastic description of the many random seeming symptoms and effects of M.E., particularly the anxiety issue, which resonates with me. M.E. is a DEPRESSING illness, not a DEPRESSIVE illness and of course, when you are in it, you don’t know if you are ever going to get better. I have been working with a practitioner of functional medicine for a couple of years and am working on diet, gut issues (a paleo diet) and stress management(mindfulness meditation), heavy metal detox (via a FIR sauna) and dampening down the fight/flight mechanism. This is a great interview and Dan asks… Read more »
Thanks for your comments 🙂
Glad the interview resonated with you – yes, so true about M.E. being depressive.
Sounds like you are on track with your recovery action plan – hope to share your story one day soon. 🙂
Wonderful and inspiring! Acceptance is key while at the same time never give up that recovery is possible. After personally living with ME/CFS for these past 18 yrs, through relapses, periods of full or part recovery, numerous come and go symtpoms, all the ups and downs of life, trying numerous ‘treatments’…..in the end the things that work for me is acceptance, letting negative thoughts wander in my brain but not focus on them so they wander out again, pacing, healthy diet and a few supplements to help manage symptoms if I need to. Of course, sometimes I wonder if I… Read more »
Great to hear Karin
It sounds like you are doing many good things – seek to expand your strategies and focus on what works for you!
Thanks for your comment. 🙂
Thanks Dan and Stuart, always good to hear recovery stories, my take away is the importance of trying to reduce stress, be positive, accept your life has to change and use pacing to rebuild appropriately
Great summary Heather – that was my take away from the interview too! 🙂
Thank you Dan and Stuart for a very helpful and enlightening interview. So pleased the pacing worked. Still trying to “master” the art myself.(As a housewife there’s always something to do!) But I have found the use of a stop watch and some self discipline helpful in this respect. It does make a difference too when there is support from someone close. I think love is the operative word here. Stuart’s cheerful countenance comes across and that is really good when you need encouragement. Feeling better myself of late but I can remember and identify with his downside. This positive… Read more »
Thanks for your lovely comment Christine. ?
Indeed, there is always something to do, it’s about prioritising and balancing your longer term needs against your short-term needs. 🙂
Hi,
Thanks to both of you for this inspiring interview.
I’m part of the program ANS rewire and a question keep coming to me after watching this. Daniel, I would be glad to read your thoughts. Why would Stuart relapse when he felt recovered? For me it’s because maybe he has a stressful work environment that he learn to manage. Another reason is maybe he went too hard too soon when he felt better.
Best. Max.
Hi Max A good question, here is my take on it. I don’t believe that Stuart was recovered until the end. He had simply reduced his stressors to such an extent that it allowed his body to somewhat return to health because it wasn’t being triggered into flare-ups all the time. The issue was that work was a very significant stressor for him, keeping his nervous system sensitised. So with ANS dysfunction remaining, as soon as he exerted himself, he of course got sick. Once he stopped work, he was rapidly able to transform his experience into a full and… Read more »
Thanks a lot Daniel. It makes sense to me now 🙂 Max.
Thanks for this Interview. I have a similar experience, als had 2-3 times where I recovered or was at 80-90% but I’m also not that bright… 🙂 Directly started with training, gym etc Sadly at that time, I didn’t knew that I have cfs, doctors just calling it depression and pushed me to do sport etc Than things get very worth and now I’m sick as never before. Bur I now know what is all about and starting now my lasting recovery, hopefully I’m sometime be able to share my story too. 🙂 But that is not for what I… Read more »
Thanks for your kind comments Marius.
Hopefully CFS Unravelled is heping you understand how and why these recoveries happen – you will hear the themes coming through in the recovery interviews!
Thank you to both of you for this interview. I’m trying to navigate my way through this confusing illness and your words have made me feel a little better informed and significantly less alone.
Thanks `Stuart and Dan for sharing this. I always find it extra encouraging when I hear of someone close to my own age who has recovered.