Living with chronic illness is difficult enough without the additional burdens of experiencing an invisible illness.
So in this article we will talk about what invisible illness really is, why invisible illness has such a negative impact on you and why it is so important to get past the injustices of invisible illnesses and how to do that.
Living with chronic illness is difficult enough without the additional burdens of experiencing an invisible illness.
So in this article we will talk about what invisible illness really is, why invisible illness has such a negative impact on you and why it is so important to get past the injustices of invisible illnesses and how to do that.
Exactly what is invisible illness?
Invisible illness is a term used to describe any medical condition that isn’t externally visible. This includes illnesses like fibromyalgia and ME/CFS as well mental illnesses and conditions like chronic migraines or chronic pain.
Some people include conditions like diabetes, Lupus or arthritis as invisible illness, however, such conditions can at least be more easily medically verified with tests. But true invisible illnesses usually evolve around symptoms like fatigue, pain and other neurological symptoms that cannot be externally measured or verified easily.
People experiencing invisible illness are often judged or unfairly criticized because they don’t look sick and are often labelled as faking illness or being hypochondriacs.
Hence the level of illness is often judged externally solely by people’s behaviour, but because most chronic illness fluctuates in severity, this leads to additional scepticism and stigma.
3 reasons why invisible illness can increase suffering
Invisible illness is like any chronic illness is already physical and mentally challenging. Besides the obvious physical and emotional suffering, people often become socially isolated and miss out on career opportunities, relationships and recreation.
But there are a number of ways people with invisible illness suffer even more than those with other chronic illnesses:
1.) Invisible illness is exhausting to explain
Being chronically ill makes everything you do more difficult. The things healthy people take for granted like going shopping or tidying up the house or even basic things like personal hygiene are often an ordeal for people with chronic illness.
This leads to many pressures including issues around social occasions, relationships and other day to day events.
Dealing with the symptoms of invisible illness is already very difficult and many people struggle to cope. However, with people often not showing understanding, make allowances or acting like there is nothing wrong with you, precious energy is wasted explaining oneself over and over again, having to reassert that they are actually ill.

This leads to many pressures including issues around social occasions, relationships and other day to day events.
Dealing with the symptoms of invisible illness is already very difficult and many people struggle to cope. However, with people often not showing understanding, make allowances or acting like there is nothing wrong with you, precious energy is wasted explaining oneself over and over again, having to reassert that they are actually ill.

2.) Invisible illness often leads to abuse
Abuse may seem like a strong word, but that is exactly what many people with invisible illness experience.
People get accused of faking their symptoms, seeking attention or being weak minded.
Because there is a lack of empathy, people sometimes also act insensitive to people experiencing invisible illness, excluding them from activities or social occasions because in the past, they have often not shown up.
Of course, chronically ill folk don't act their best, but instead of showing understanding, people often label those with invisible illness as being unreliable, lazy, tardy or other negative qualities.
3.) Invisible illness often leads to negative emotions
Yes, people with chronic illness will already experience negative emotions such as feelings of frustration, loss, loneliness and sadness that often leads to depression.
But the stigma of invisible illness often leads to additional feelings like shame, embarrassment and even guilt.
This is because of the divide caused by the lack of acknowledgement, empathy or understanding from people around them, including family, friends and sadly sometimes even health care professionals.
All these additional negative emotions need to be worked through or dealt with, adding to the burden of chronic illness.
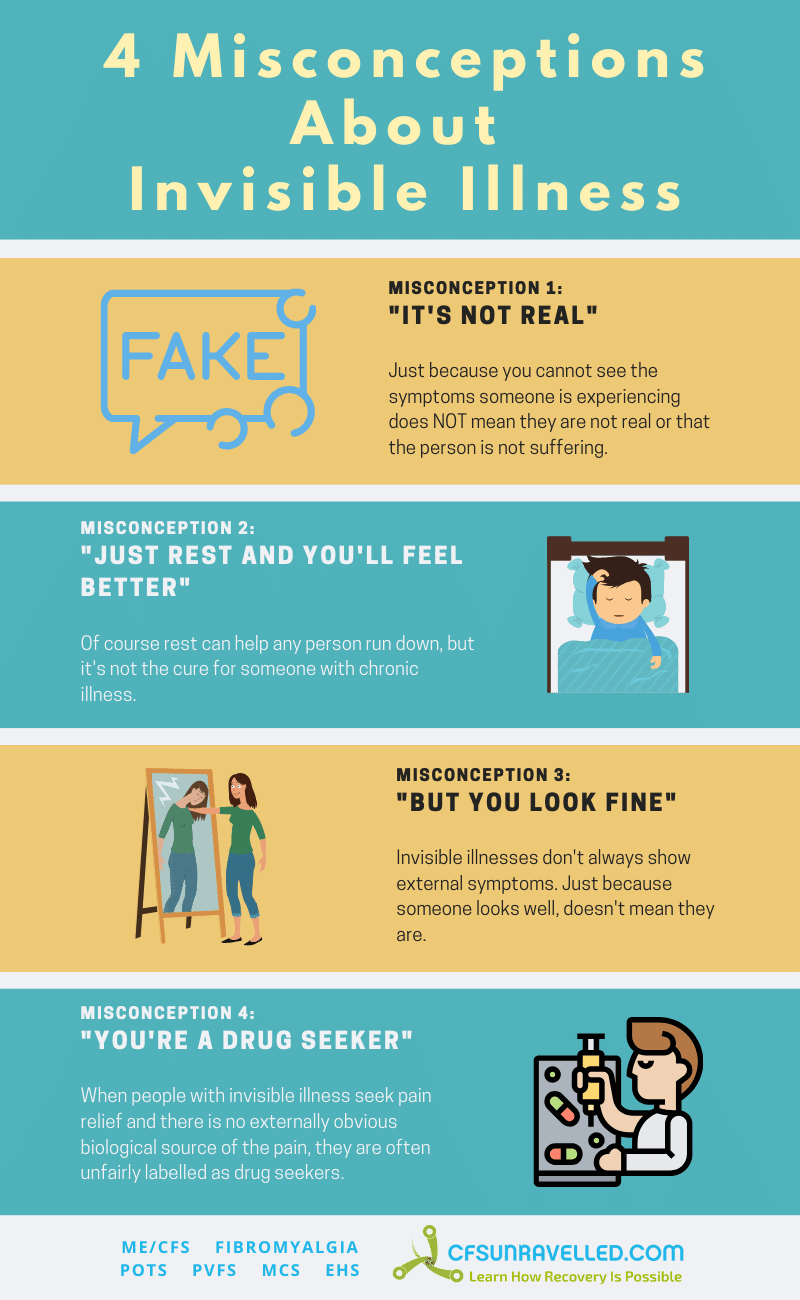
Just about everyone that experiences an invisible illness has dealt with misconceptions regarding their condition. These include:
1.) Invisible illnesses are not real or are ‘all in the person’s head.’
This ties closely to the idea of the person being a hypochondriac or that they are ‘simply’ depressed or anxious. In fact, many people with chronic illnesses experience depression and anxiety as a result of the difficulties they experience, or may even have experienced them before their chronic illness. However, that does not mean that the illness they experience isn’t real or psychological in nature. (unless of course we are talking about mental illness as invisible illness)
2.) Just rest and you’ll feel better.
This is a complicated one, because of course rest will actually often help people feel better. But often, resting doesn’t help and many people with invisible illness feel there is only so much rest a person can have. (they need to live a little too!)
What’s frustrating is that the suggestion of rest can sometimes suggest that they are ‘simply tired’, when in fact they are experiencing a disease process that is making them feel exhausted.
Share this graphic on your website!
2.) Just rest and you’ll feel better.
This is a complicated one, because of course rest will actually often help people feel better. But often, resting doesn’t help and many people with invisible illness feel there is only so much rest a person can have. (they need to live a little too!)
What’s frustrating is that the suggestion of rest can sometimes suggest that they are ‘simply tired’, when in fact they are experiencing a disease process that is making them feel exhausted.
3.) But you look fine.
It’s really at the core of invisible, you look fine so therefore you must be fine.
Of course this is difficult for anybody to understand, no matter how understanding they are. This is especially the case when the last time they saw the chronically ill person, they were able to do more and reported feeling better. When they look the same as the last time, equally well, how can they report that they are feeling so unwell now?
But you’re having a good time…
Perhaps you can see the conundrum here. When a person suffering from a chronic illness that is invisible is trying to make the most of life and enjoy themselves, people automatically assume everything is fine again.
When you have to spend all your time proving how sick you are, then even if you feel a little better you almost have to be scared to show it for fear of being dismissed next time you are feeling worse.
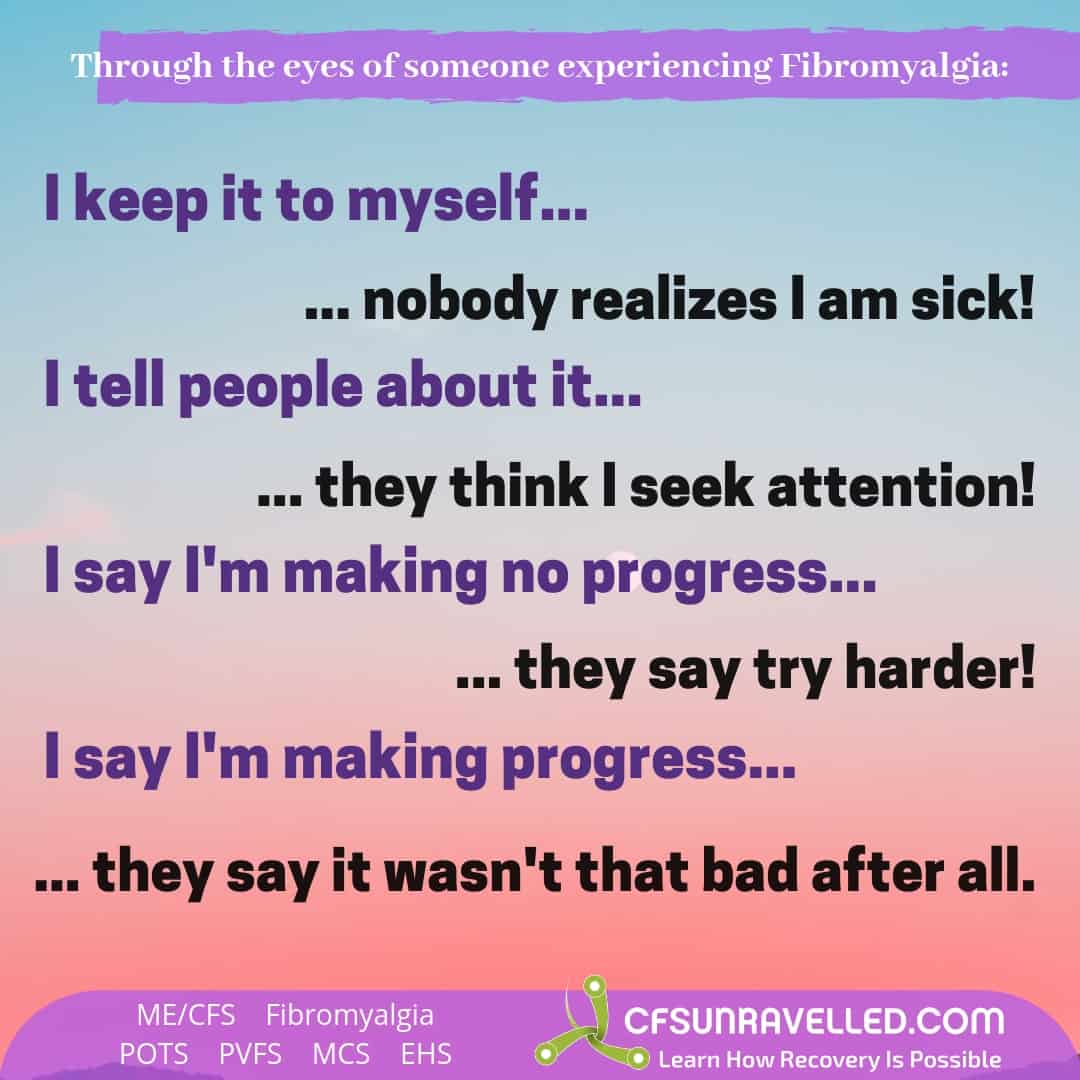
But you’re having a good time…
Perhaps you can see the conundrum here. When a person suffering from a chronic illness that is invisible is trying to make the most of life and enjoy themselves, people automatically assume everything is fine again.
When you have to spend all your time proving how sick you are, then even if you feel a little better you almost have to be scared to show it for fear of being dismissed next time you are feeling worse.
4.) You’re a drug seeker…
That’s the problem with invisible symptoms like pain. When there is an obvious physical diagnosable cause of pain, people show understanding. But in chronic pain there often isn’t such an obvious connection and people’s calls for help is often translated as them being ‘a drug seekers’.
Points 3 and 4 above lead us to perhaps the worst aspect of invisible illness:
The worst impact of invisible illness – it’s not just the injustice of it all
Yes, there are many emotionally painful aspects of dealing with an invisible illness, but perhaps the worst aspect is how it affects people’s ability to move forward and cope with and overcome their illness.
Impact of negative emotions on people experiencing invisible illness
It doesn’t take a rocket scientist to work out that experiencing ongoing negative emotions as described above is going to have an impact on your mental health and can lead to anxiety and depression.
But research has shown that stress also impacts other chronic illnesses including those with more obvious and measurable symptoms such as Irritable Bowel Syndrome. One study show how the perceived stigma of invisible illness in patients may lead to significantly worse outcomes. 1
The negative and positive impacts of emotion on chronic pain perception are already well understood with much medical research in this area. 2
Whilst the impact of stress is probably is felt by most people with chronic illness, for people experiencing ME/CFS, Fibromyalgia, POTS and related syndromes it is often even more obvious. When physical stress, such as exercising, lack of sleep or even eating certain foods such as sugar and alcohol, flare ups often follow. But most people will also notice that if they experience mental stress such as working too long or studying too hard, or even psychological or emotional stresses occur, that their symptoms worsen and lead to flare-ups.
Reduced treatment seeking and reduced treatment access
Let’s face it, few things could be more important than getting treatments to help you feel better when you are chronically ill.
But the stigma of invisible illness often makes people feel like they look like malingerers, hypochondriacs or that they are weak, making them not speak out and seek help. Research has show how fibromyalgia patients battle for symptom legitimacy and how there is very real scepticism about illness like Fibromyalgia by many physicians. 3
Now obviously people can experience additional negative health conditions, and if they stop seek medical advice, the impacts could be tragic.
But even if we put aside the seeking or not seeking of medical assistance (and we probably shouldn’t), then even the simple fact of putting all your limited energy into wrestling with this whole debacle of invisible illness could waste valuable resources. Resources that you could put towards coping with the illness, lifestyle adjustments to manage your condition and squeezing whatever happiness you can out of life.
Clearly, the negative impacts of invisible illness are much more than just an annoyance, then can be a very real obstacle towards better physical and mental health.
How to support others with invisible illness – 6 Key steps
1.) Get your support into the right perspective
For many people, it is a natural instinct to come to the rescue when a loved one is dealing with a health crisis. But if your loved is experiencing an invisible illness like ME/CFS, Fibromyalgia, POTS or MCS, there is no silver bullet cure for you to give to them.
That doesn’t mean you can’t support them to regain their health with a partial or full recovery, but supporting the person experiencing invisible illness is often as much about their emotional well being as it is their physical well being. It is about supporting them so that they can take positive actions towards their recovery.
2.) Make their invisible illness seen
One of the biggest frustrations with invisible illness is when people don’t believe you. Loved ones often feel like downplaying the person’s symptoms or severity, because they don’t want them to suffer, they want to uplift them.
But it often has the opposite effect because the ill person then has to spend their limited energy explaining and justifying their experience in an attempt to feel validate.
So validate them. Acknowledge their symptoms, the severity and their suffering – just listen and show that you believe them.
By taking a little time to learn about the illness, you will be able to recognise signs of their symptoms. This in turn will allow you to acknowledge them more effectively. You don’t have to become an expert, but knowing some of the basics is key as it can help you to remind the person what is normal and what is not.
3.) Keep it positive
Once you have shown that you believe and acknowledge the invisible illness, then you can gently help the person develop a positive attitude or look for some kind of positive focus or distraction.
Always talking about the illness and the symptoms is not helpful, and usually driven by not being believed and/or seeing any way to resolve the illness.
By first acknowledging and validating their invisible illness and suffering as real, and then finding even a single small action to improve their daily experience, we can often find the space to shift the focus onto something more positive to give the person experiencing the illness some mental respite.
4.) Respect their boundaries
Dealing with any chronic illness, not just invisible illness, is not always easy to cope with. Part of coping sometimes means to withdraw whilst dealing with the challenges.
People with invisible illness often lose a lot, connection to family and friends, exercise, sports, other social activities and so on. Nudging them to keep some connections where possible makes sense, but it’s important to recognise and respect their boundaries and respect their decision to withdraw when they feel the need.
5.) Look after yourself
That might sound surprising, but it’s really important not to become a martyr and to demonstrate some good self-care. Missing out on everything because your partner or family member has invisible illness isn’t helpful – it just adds to the guilt they are experiencing. Be sensitive about sharing some of your ups, but don’t stop experiencing them.
Looking after yourself also means that you will be better able to support the person experiencing invisible illness. It can be wearing to support someone with chronic illness, which can lead to short fuses, insensitive responses and not showing the kind of sensitivity and support that you want to. The best way to avoid this, is to look after yourself and give yourself a break from invisible illness when you can.
6.) Keep it real
It’s all too easy to start treating someone like an invalid when they are dealing with a chronic illness. To look at them like they this victim, where nothing exists but their suffering.
Well, people with invisible illness often do feel like that, but you treating them like that doesn’t help.
So make sure you remember that this is the same person you knew before they got ill. If you have only known them ill, then seek to see that there is much more to them then a shell of a chronically ill person.
Be sensitive and kind. Show compassion and patience. Don’t judge but show empathy. Don’t treat them with kid gloves the whole time, help them connect to feeling like a normal person, even if they’re not.
7 Ways you can learn how to cope with invisible illness
Knowing how to cope with invisible illness can be difficult. Not only do you need to cope with chronic illness, but you also need to manage the issues around people not understanding or believing what you are going through.
Here are some helpful strategies to help you cope with invisible illness:
1.) Acceptance – don’t be worse to yourself than everyone else
When people experience the injustices of invisible illness, they often get frustrated, sad and even angry. But a real question to ask yourself is; “Are you demonstrating belief in your invisible illness?”.
Many people that come down with invisible illness seek to keep up appearances due to feelings of shame or lack of a clear explanation for their symptoms. They often don't realise just how much the illness is impacting them.
Accepting the symptoms as real, accepting that you are ill and making adjustments to how you try to engage with life is key to reduce your suffering.
Many people simply try to push on and live life as though they are not chronically ill, causing huge amounts of stress leading to exacerbation of both physical and mental symptoms.
So it is about letting go of expectations of what ‘should’, ‘needs to’ or ‘must’ happen. Seek to develop a more flexible approach towards life. Seek to ‘take it as it comes’.
2.) Become your own advocate & become a self-manager
When we are vulnerable and ill, we often hope that someone will rescue us, will fix us. Many people keep seeking that person or that solution that will suddenly make it all go away.
Of course it makes absolute sense to keep seeking solutions and answers, but what is key is that you take ownership and responsibility for your outcomes.
Often you will hear people say in recovery interviews that they suddenly realised it was up to them to find the answer and solution and that this is the point things turned around for them.
So keep accurate records of your treatment and symptom timelines and that you have copies of test results so that when you see a new doctor, that you can present the information in a coherent and succinct way.
Being your own advocate also is about standing up for yourself. This isn’t always easy, especially if you don’t fee well. Often it about biding your time, waiting for the right time where you are able to have those important discussions with people. Many of us often feel short of doing a good job here, and that’s OK, but at least have it in the forefront of your mind to become a strong advocate for yourself and speak up about the help you needed and how people treat you.
3.) Focus on your mental health as much as your physical health
Yes, you may feel anxious, you may feel depressed – it’s to be expected when dealing with invisible illness or any severe chronic illness.
But it’s all too easy to simply say to yourself, when I am no longer physically ill, then I can be happy.
Physical and mental health are ultimately connected, but it’s really important to prioritise your mental well-being first and foremost because it is the lens through which you experience life.
So seek to get help and find resources and strategies to help you stay mentally as healthy and strong as possible. This is key to help you move forward in all aspects of your life, including your efforts for recovery from invisible illness.
One of the most important things you can do is to stop wasting your energy on things you cannot control, like people who simply don't understand you. So stop doing things that drain you when you have invisible illness, it's not worth your energy.
4.) Find a way to escape from invisible illness
The real problem with chronic illness is just that; it’s chronic. That’s wearing, it’s tiring and without any kind of respite, our resilience can diminish.
Ultimately, you of course can’t put invisible illness on hold or magically make it go away for a few hours. But you can do your very best, no matter how difficult it is, to find something else to engage your mind and your spirit for a short time.
Maybe it’s your favourite TV show, maybe it’s a hobby you can engage in in a limited way or maybe it’s just finding the joy in a moment as it presents itself. Look out for the little blessings in your life and find a way of enjoying even the smallest pleasures.
5.) Surround yourself with positive people
Everyone is affected by the people they have around them, but perhaps chronically ill people even more so. (who has the energy to resist, right?)
You know how some people pull you down and some uplift you. Some are downright energy suckers, whilst others pull you down even though they mean well.
Sometimes having somebody a little less empathetic with a positive bubbly attitude can be just what the doctor ordered (in small quantities).
Invisible illness is often a lonely experience, so we cling onto whatever or whoever we can. But it’s important to reflect if those interactions are uplifting you or pulling you down. If you make changes, do so subtly, the last thing you need is drama or conflict.
6.) Dip into chronic illness communities to gain strength in numbers.
There is nothing like not feeling alone to really help you feel validated. Interacting with others that have the same challenges with invisible illness as yourself can be a real relief; “see I’m not the only one, I’m not making it up”.
But remember the above point about surrounding yourself with positive people. Whilst some chronic illness support groups can be positive and supportive, others can be downright toxic. So stay away from negative spaces and even limited your connection to positive chronic illness communities.
Whilst it’s fine to help others and uplift them at times, it’s more important for you to look after yourself and not allow yourself to be dragged down. So be mindful of these interactions.
7.) Dare to dream
Chronically ill people often resign themselves to staying ill when there are no obvious solutions to cure them. That makes sense, right?
However, I have found that the people who dare to dream of more positive times, dare to dream of some experiences that are out of reach right now, often do better.
The key is not to attach a huge emotional load to such dreams. If not experiencing that dream would crush you, then it’s not the right dream!
Ideally it’s a mix of things;
- some dreams that seem possible, perhaps just out of reach;
- some dreams that would be amazing, but not so easily attainable.
Having that mix helps you keep the fire burning, because when the ‘just out of reach’ dreams happen, you can’t help whether the other dreams may be possible too. The key for recovery from chronic illness is often not finding some magic cure or becoming fully recovered, but rather just being a little more recovered. Think progress, not perfection.
Citations:
1.) Rhudy, J. L., & Meagher, M. W. (2001). The role of emotion in pain modulation. 14(3), 241-245. Retrieved from https://journals.lww.com/co-psychiatry/Abstract/2001/05000/The_role_of_emotion_in_pain_modulation.12.aspx ⤣
2.) Taft, T. H., Keefer, L., Leonhard, C., & Nealon-Woods, M. (2009, August 1). Impact of Perceived Stigma on Inflammatory Bowel Disease Patient Outcomes. Inflammatory Bowel Diseases, 15(8), 1224–1232. Retrieved from https://doi.org/10.1002/ibd.20864 ⤣
3.) Wolfe, F. (2009, Apr). Fibromyalgia Wars. The Journal of Rheumatology, 36(4), 671-678. Retrieved from https://doi.org/10.3899/jrheum.081180 ⤣

There is a lot of good content in here, I remember feeling bad that whenever people would ask how I was I felt I had to say ‘good’, but really I felt crap, but when you did say you felt crap, there was that assumption which you mention, that a rest would help me feel better, but in fact, I never felt better. I am so glad those days are behind me, the burden of carrying an invisible chronic illness is profound, and exhausting, and sometimes now I still feel a wave of tenderness to my past self, to see… Read more »
Hi Heather
“waves of tenderness to my past self” – yes that resonates and was reflected in my previous blog: https://cfsunravelled.com/how-mecfs-fibromyalgia-really-affects-you-even-those-experiencing-dont-know/
Thanks for sharing your thoughts.
I’ve had to disconnect from a friend who kept asking me why I “avoid” social occasions, or don’t always join in when I do attend. I explain it’s the waves of total exhaustion one experiences with fibromyalgia but she keeps telling me “We all get tired as we get older, you need to overcome it like me!” I also receive abuse about my Christian faith because they can’t see the invisible illness, so it must be my faith that “stops me having fun”, especially as alcohol has an adverse effect on me, so I rarely drink, and then scantily. I’m… Read more »
It’s just too hard with some people – I totally get it.
You have to focus on yourself above all else.
As you progress with your recovery, all these things get easier.
Hey Dan. Thanks for this post, thats what i needed this time. For me, its meanwhile the most frustrating thing with CFS. I gained massive health, compared to my badest time, i can walk up to 20.000 steps per day, 10.000 in the morning, 10.000 in the evening. Lost over 120 pounds, can watch TV again… thanks to your book/website. (And Gupta) But have a lot to do, before im really recovered to 100%. And thats lead to my question… Short before corona i moved into another city, wanted to give my life a new start,all alone. So, then im… Read more »
Hi Michi I am so sorry for your experience – I think most people with this illness can relate to your pain here! Look, the key in my experience is to stop seeking that approval from others. Once you realise they are ignorant (mostly not malicious), it’s much easier to let it go. If you spoke to 6 year old who said “you are silly for wearing flippers in the pool, you’re not supposed to wear shoes whilst swimming and these look so silly”, then you would not be thinking about it years later. We all make the mistake of… Read more »
Thank you so much Dan for the time you give to us to share your wisdom, your knowledge ,and your compassion. I so very much appreciate it all and find it most encouraging and hopeful. Please know your support and encouragement is much needed. Thank you!
Great to hear Dianne.
Hope you are enjoying the recovery stories and other blog posts about recovery.